House Republicans are advancing a new budget proposal that would tie Medicaid eligibility for certain adults to mandatory work or community engagement, reigniting a national debate over health coverage and employment.
The plan targets able-bodied adults without dependents, aiming to require them to complete a fixed number of hours in approved activities such as employment, education, or volunteering to maintain access to the program.
According to Newsweek, this effort mirrors earlier policies attempted during the Trump administration and has drawn sharp criticism from public health experts and policy analysts who warn it could result in widespread coverage loss and increased administrative costs.
Proposed Policy Would Require 80 Hours of Activity for Able-Bodied Adults
The legislation under review by the House Committee on Energy and Commerce would require able-bodied adults aged 19 to 55 without dependents to complete at least 80 hours per month of verified work, education, or volunteer activities to maintain Medicaid eligibility.
The bill is part of a broader reconciliation package passed by the House in April.
The law also seeks to reduce the Department of Health and Human Services budget by $880 billion over ten years, with major implications for state Medicaid funding and federal responsibilities.
According to the Congressional Budget Office (CBO), the proposal would save the federal government $109 billion over a decade but result in about 600,000 individuals losing coverage.
It would also shift $65 billion in costs to state governments and reduce the federal match rate for Medicaid expansion from 90% to a range between 50% and 83%.
Critics and Supporters Present Diverging Views on Impacts
Proponents of the reform argue it would encourage employment, deter fraudulent enrollment, and promote self-sufficiency among recipients.
Opponents counter that such policies add bureaucratic barriers and risk removing coverage from qualified individuals.
Dr. Susan Dorr Goold of the University of Michigan told Newsweek:
“They seem logical, but most able-bodied Medicaid enrollees already work. Sometimes their employment is not reliable, for example, in restaurants or tourism.”
“The data show that work requirements increase costs by adding bureaucracy, have no effect on employment, and disenroll eligible people who don’t navigate the bureaucratic requirements correctly.”
Jamila Michener, Associate Professor of Government and Public Policy at Cornell University, also criticized the policy:
“Medicaid work reporting requirements are an ineffective policy mechanism that achieves little except to create barriers to healthcare access.”
“Work requirements have already proven to be a failed policy that produce no discernable benefit.”
“There is growing evidence of the harms of work reporting requirements including cutting off access to health care, driving up uninsured rates, increasing the burden of medical debt, and a range of other adverse consequences.”
“Work reporting requirements create administrative burdens for already vulnerable populations. They also create confusion and unwarranted disenrollment from Medicaid, as people often don’t know about them, causing perfectly eligible beneficiaries to lose benefits simply due to lack of information.”
Michener further noted that the harms are disproportionately experienced by Black Medicaid beneficiaries, adding a racial equity dimension to the debate.
Georgia Leads Implementation, Other States Seek Federal Approval
As of now, Georgia is the only state with a federally approved Medicaid work requirement. The policy was implemented in July 2023 and is set to expire in September 2025, though the state has announced its intent to seek an extension.
Under Georgia’s model, Medicaid applicants must complete a minimum of 80 hours of community engagement activities before coverage begins.
Several other states are actively seeking federal approval for similar programs.
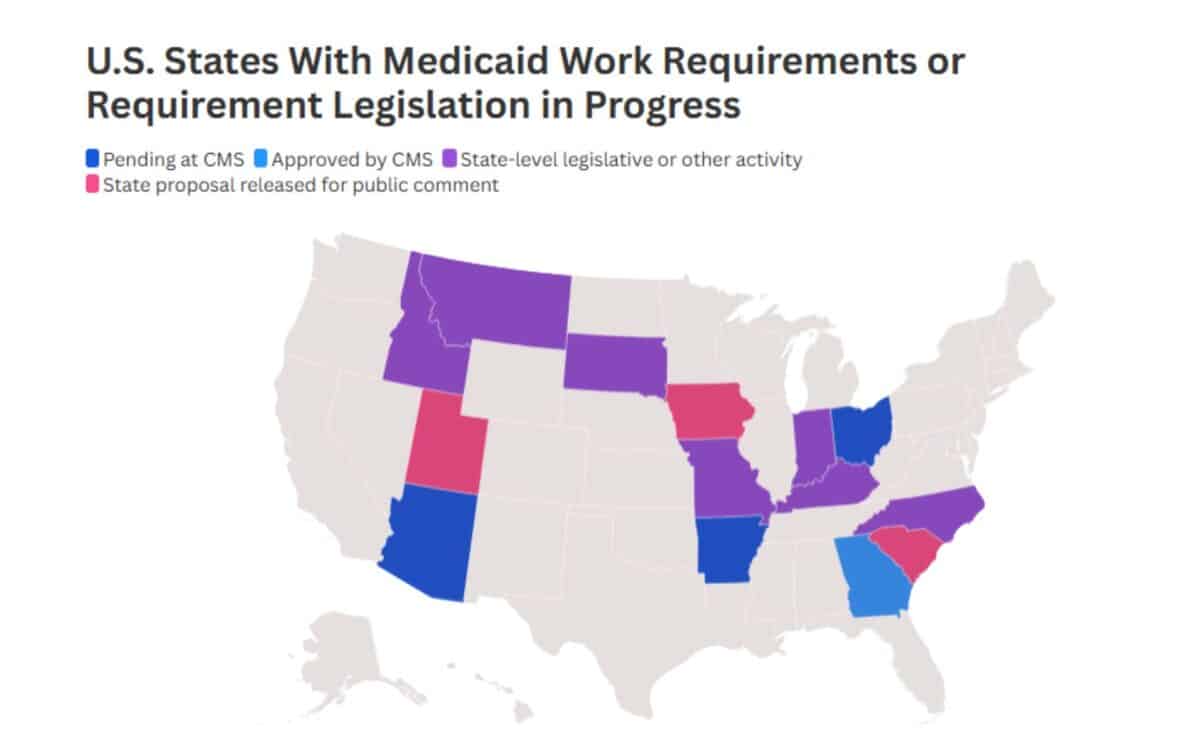
In Arizona, the proposal would require individuals to engage in at least 20 hours per week of work or related activity, and introduces a one-year coverage ban for those who knowingly provide false income information or fail to report changes.
Arkansas is pursuing a system in which beneficiaries would be assessed as either “on track” or “not on track” toward meeting personal health and economic goals.
The state previously implemented work requirements in 2018, which led to 18,000 people losing coverage before courts determined the policy violated Medicaid’s mission.
Ohio has also submitted a new 1115 waiver that would make Medicaid expansion coverage conditional on meeting work requirements.
Legislative Activity in Multiple States
In addition to Georgia, several other states are progressing through legislative or regulatory processes:
- Idaho, Indiana, and Kentucky have already passed legislation requesting federal approval for Medicaid work requirements.
- Missouri is awaiting state Senate approval for a similar bill.
- Montana‘s governor has signed a law to pursue a federal waiver.
- Legislative processes are also underway in North Carolina and South Dakota.
Public Comment Periods Underway
Some states remain at the public consultation stage of the process. In Iowa, the comment period is open until May 15. In Utah, it will close on May 22, and in South Carolina, the period continues until May 31.
Each of these states is seeking to amend its existing Medicaid policies to introduce or expand work-related conditions as a requirement for coverage.
The federal legislation also includes new administrative provisions aimed at tightening eligibility enforcement.
Among them are semi-annual income verification checks, replacing the current annual review process, and cost-sharing measures that would require some enrollees to pay more out-of-pocket for care.
These reforms are intended to strengthen oversight and reduce long-term federal expenditures.